Continued….
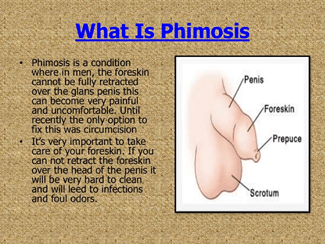
Phimosis is a condition in which the prepuce cannot be retracted over the glans penis. It could be further defined as physiologic, as in infancy and childhood, or pathologic. Pathologic phimosis would result from inflammatory or traumatic injury to the prepuce resulting in an acquired inelastic scar that prevents retraction. Forceful disruption of physiologic adhesions in infants no doubt encourages pathologic phimosis. Physiologic phimosis is common in male patients up to 3 years of age, but often extends into older age groups.
Homoeopathic Treatment—Merc. Cor. 6—If the fore-skin is fissured. Rhus Tox. 3—If the fore-skin itches or is inflamed. Cannabis 3x—If the skin is inflamed, red and swollen.
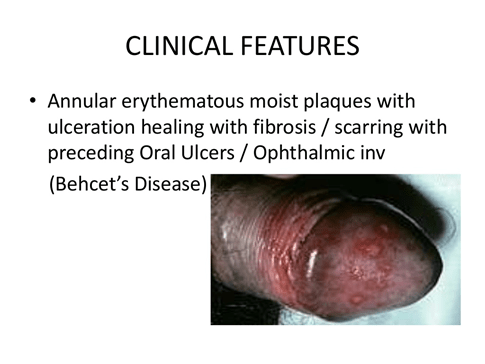
Balanoposthitis:
Balanitis is the term for inflammation of the glans penis. Posthitis is defined as inflammation of the prepuce.
Balanoposthitis is inflammation of both It is fairly common, occurring in 4–11% of uncircumcised boys.
The etiology is unclear and no cause can be identified in many cases, although infection, mechanical trauma, contact irritation, and contact allergy are cited.
Management of balanoposthitis includes improved hygiene with gentle foreskin retraction, sitz baths, and cleaning of the foreskin.Topical ointment and oral antibiotics are indicated for suspected acute bacterial balanoposthitis. Because Group A beta hemolytic streptococcus is a common bacterial cause of balanoposthitis, first-generation cephalosporins or penicillins have been typically recommended.
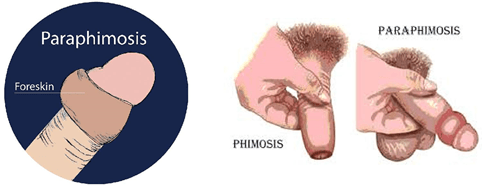
Paraphimosis:
Paraphimosis is a condition in which the foreskin is left retracted because of entrapment of the tight prepuce proximal to the corona,ie: the round elevated part.
The glans engorges and the prepuce becomes edematous because of lymphatic and venous congestion. Thiscould happen because boys have been encouraged to retract the foreskin for physiological phimosis by parents or medical staff. In most instances,manual compression can reduce the preputial edema within the first few hours. In difficult cases, various techniques are described, including applying granulated sugar to the penis, adding multiple punctures to the edematous foreskin before compression, injecting hyaluronidase beneath the narrow band to release it, and wrapping the distal penis in a saline solution–soaked gauze swab and squeezing gently but firmly for 5–10 min. Thereafter, physicians are supposed to push forcefully on the glans with the thumbs, while pulling the foreskin with the fingers. However, an emergency dorsal slit may be necessary in late cases. Some authors advise circumcision for paraphimosis because of its tendency to recur,whereas others insist that circumcision is not mandatory because the foreskin will continue to develop normally.
Inability to draw back the fore-skin which has once been drawn up, Colocynth is indicated. Aconite, Belladonna and Nux vom are also indicated with acute symptoms and in emergency till advanced care is provided.
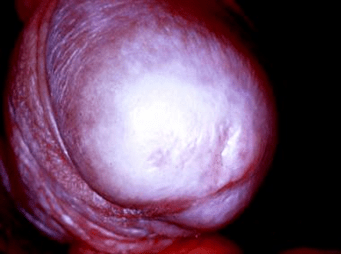
Balanitis Xerotica Obliterans:
Balanitis xerotica obliterans (BXO), known as lichen sclerosus, is an infiltrative skin condition that causes a true phimosis and a clinically recognizable lesion at the tip of the prepuce. It is usually distinguished by a ring of hardened tissue with extensive scarring, a whitish color at the tip of the foreskin, and edema. It has been said to be a common underlying cause of persistent nonretractability of the foreskin at puberty, while the overt lesion is rarely seen in children under 5 years of age. However, BXO was found in 15% of children undergoing circumcision for phimosis. Presentation is with inability to retract the prepuce, discomfort after micturition, and occasional minor obstructive signs. The preferred treatment for BXO has been circumcision, which will remove all the affected tissue. Preputioplasty is not an option because the continuing inflammatory process results in recurrent stenosis of the preputial orifice. Remaining lesions on the glans nearly always regress or resolve following circumcision. Meatotomy or meatoplasty is needed in cases of severe meatal involvement,and postoperative application of topical steroid may lessen the risk of subsequent restenosis.
Homoeopathic treatment: Merc sol, Borax, Argentum nitricum, Syphilinum, Nitric acid , Thuja and many more medicines as per indications.
Homeopathy medicines have a powerful anti-inflammatory effect which treat the infection from the root, prevent further recurrences, prevent complications and saves you from a surgeon’s knife.
A study carried out at Bristol Homeopathic Hospital, UK, has revealed that more than 70% of patients with chronic diseases said homeopathy helped them feel better. The 6-year study involved over 6,500 patients.
There are 65 homeopathy medicines which give great relief in balanitis / balanoposthitis / infected head of penis. However, the correct choice and the resulting relief is a matter of experience and right judgment on the part of the doctor. The treatment is decided after thorough case taking of the patient. Thus remedies are tailor made as per the individual case.
CIRCUMCISION:
Circumcision as Religion and Rite of Passage Globally, most circumcisions are performed for religious reasons and are a fundamental part of the Jewish and Muslim faiths.In the Jewish belief,circumcision is a covenant between God and Abraham, as written in the Bible(Genesis) and should be performed by a mohel when the boy is 8 days old.
Muslim society considers it a tradition of the Prophet Mohammed (Sunnah) to introduce the boy into the religious Islamic community, although it is not mentioned in the Holy Koran.
Male circumcision that is performed for any reason other than physical,clinical need is termed nontherapeutic (or sometimes ritual) circumcision.
Circumcision that is performed for any reason other than physical,clinical need is termed nontherapeutic (or sometimes ritual) circumcision.
Circumcision as Prophylactic Therapy:
Prophylactic Circumcision to Prevent Urinary Tract Infection(UTI):
Incomplete preputial separation has been considered responsible for colonization of the prepuce by pathogens, which leads to balanoposthitis or UTI. The incidence of UTI has been reported to be lower in circumcised than uncircumcised infants. An unretractable prepuce has been considered responsible for colonization of the prepuce by pathogens, which leads to UTI. An association between a decreased incidence of UTI and circumcision during the first year of life has been reported.
Prophylactic Circumcision to Prevent Sexually Transmitted Infection(STI)
Whether early childhood circumcision reduces the risk of future STIs other than human immunodeficiency virus (HIV)has been controversial. In 1998, Moses et al.analyzed studied and reported a strong association between the lack of circumcision and chancroid, syphilis, genital herpes,and gonorrhea, but no association with urethritis other than gonorrhea and genital warts. Reports showed that circumcised men are at low risk of chancroid and syphilis,but there is less association with herpes simplex type 2.
Prophylactic Circumcision to Prevent Human Immunodeficiency Virus (HIV)
In Africa three RCTs were abandoned before their designed completion because of significant reductions in HIV incidence in the circumcised groups. Lack of circumcision has long been recognized as a risk factor for HIV acquisition in heterosexual men. This makes biological sense because superficial Langerhans cells, which express HIV-1 receptors, are more prevalent in the male foreskin than in the remainder of the penis. Additionally, decreased keratinization of the foreskin increases susceptibility to minor trauma during intercourse, potentially aiding the passage of HIV.
According to WHO and UN AIDS programme models, The models predicted that one new HIV infection would be averted for every 5–15 men newly circumcised.
Prophylactic Circumcision to Prevent Penile Cancer
Incidence of carcinoma of the penis varies greatly with the standards of hygiene, and the religious and cultural practices of different countries. It is usually seen in men who have poor standards of penile hygiene. In men who have not been circumcised, tumor development has been attributed to the chronic irritative effects of smegma, a by-product of bacterial action on desquamated cells within the preputial sac. Closed preputial sacs promote development of penile carcinoma by a carcinogen. Smegma has been implicated as the carcinogenic agent and although definite evidence has not been established, its association with the development of penile cancer has been widely observed.
Phimosis is present in 25–75% of patients with penile carcinoma.
The true incidence of phimosis might be even higher, since information about its presence is not available in many patients in whom the prepuce has been destroyed by the tumor. Circumcision protects against penile carcinoma and is a well-established prophylactic measure that almost eliminates the occurrence of penile cancer. Neonatal circumcision is done for all Jewish males and carcinoma of the penis is almost nonexistent in this population. Neonatal circumcision reduces the risk of penile cancer by at least ten times. In Muslims, who circumcise boys before puberty, penile carcinoma is rare. Adult circumcision does not offer protection from subsequent development of disease, suggesting that some period of exposure to smegma might be necessary for carcinogenesis, and accounts for the decreased effectiveness of pubertal circumcision and the negligible protective effect of adult circumcision.
METHODS OF CIRCUMCISION
Neonatal circumcision and also in older children.
ALTERNATIVE TREATMENTS TO CIRCUMCISION
Manual Retraction Therapy
Topical Steroid Therapy
Dorsal Slit
Preputioplasty:
Triple-incision or Y-V plasty.
Note: This article is for health education and awareness purpose only. Indicative homoeopathic medicines should not be taken by self prescription or on the counter. Consult the given specialist for accurate treatment.
Q. Whom to consult ?
Ans. Nephrourologist and a Homoeopath.
Q.What is the role of a homoeopath?
Ans. A homoeopath can assess the person holistically taking in to consideration all his mental, physical symptoms, the causative factors, duration and progress of the disease. The investigation reports and the nephrourologists intervention is also studied and discussed to prevent any recurrence. Many cases in early stages, the diseases were cured and in some others the surgical procedures were conducted with post operative follow up with homoeopathic medicines. Homeopathy works well post surgery to prevent complications and recurrence of symptoms too.

Hi, Thanks to this article, I have found a lot of information for my research about Homeopathy. Really have a lot of information in a different way. First time i have found this kind of article.
I would like to share some additional information about : How can homeopathy help
It will be useful for this article readers.
Thanks
Dr. Jhone
LikeLiked by 1 person
Thank you for the feedback Dr.Jhone.
Your website is quite informative too.
LikeLike